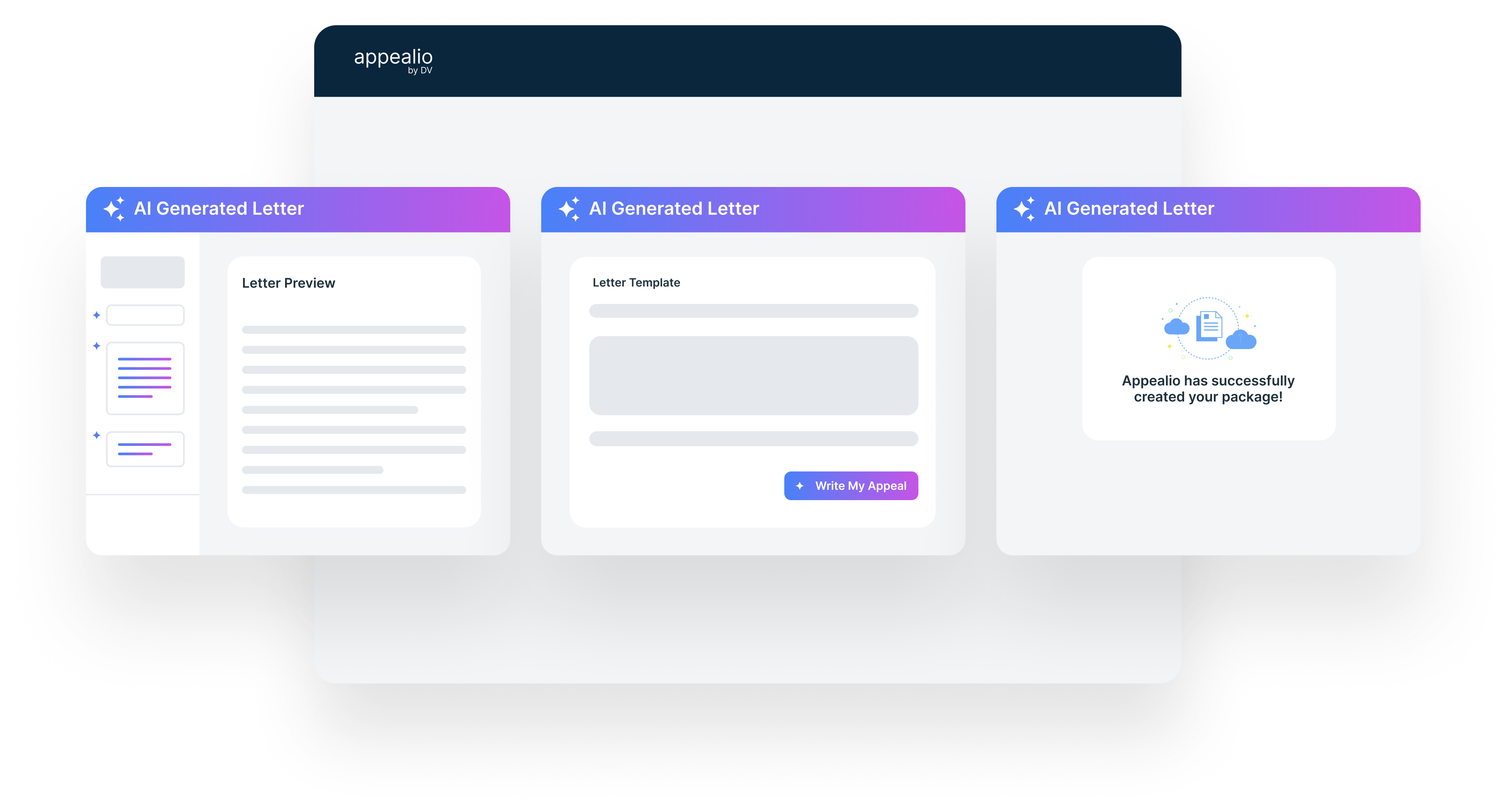
Template Intelligence: Start from your
templates or DocVocate best-practice sets to keep quality
consistent and auditable.
Policy-Aware Drafting: Auri interprets denial
reasons, coverage criteria, coding rules, and specialty
nuances to construct clear arguments.
Evidence & Citations: Pulls the right
excerpts from documentation and links to payer
policies/guidelines so every assertion is traceable.
Human-in-the-Loop: Redlines, comments, and
gated approvals keep humans in control—then hand off directly
to packet assembly and submission.